Over the recent years there have been a number of developments in the surgical management of glaucoma using minimally invasive techniques that are performed in combination with cataract surgery or as standalone procedures. These devices, such as the iStent and the Hydrus stent, are performed in the operating room under local anesthesia. These implanted devices have a very high safety profile and improve the outflow of aqueous. After implantation they are effective, in most instances, of reducing intraocular pressure and are often useful in reducing the number of eye drops needed to treat mild to moderate glaucoma.
The XEN gel stent is a small microstent that is inserted into the eye to allow for an alternative route of fluid to drain from the eye underneath the conjunctiva, which is the skin covering the eye. The XEN stent may be performed as a standalone procedure, or in combination with cataract surgery.
The procedure normally takes 10-20 minutes to perform. After the procedure patients are prescribed a topical antibiotic to be taken for 1 week and a topical steroid to be taken for 4 weeks.
The Kahook Dual Blade and the OMNI System are both devices that perform what is called a trabeculotomy. A trabeculotomy is an opening into the trabecular meshwork, which is the natural internal drainage system for aqueous fluid. This procedure increases the outflow of fluid from the eye and thereby reduces the intraocular pressure. The procedure with either device normally takes about 5-10 minutes to perform and is often performed in combination with cataract surgery. Both can, however, also be performed as a standalone procedure in patients who have not had prior cataract surgery. The OMNI procedure additionally dilates the trabecular meshwork to increase aqueous outflow.
After the Trabectome procedure, patients are prescribed a topical antibiotic for 1 week and a topical steroid for 4 weeks. Patients are also prescribed a medication called pilocarpine, which constricts the pupil, for 4 weeks.
In the most severe cases of glaucoma, where laser, medical and often other surgical procedures have failed to control intraocular pressure or in severe cases where very low intraocular pressures are needed to preserve vision, additional procedure are available and are highly successful.
Trabeculectomy is a type of glaucoma surgery performed on the eye that creates a new pathway for fluid inside the eye to be drained to a fistula created on the surface of the eye. This is an outpatient procedure performed in the operating room. It is used to prevent worsening of vision loss due to glaucoma by lowering eye pressure.
After trabeculectomy, patients prescribed a topical antibiotic for 1-2 weeks and a topic steroid for 4 weeks.
Glaucoma shunt insertion is a surgical procedure that creates an alternative route for fluid to get out of the eye. Glaucoma shunt insertion is often performed after medical and laser treatments are unsuccessful at controlling the glaucoma. Compared to a trabeculectomy, glaucoma shunt insertion inserts a shunt into the eye to drain fluid to an extraocular reservoir that is covered by the conjunctiva, which is the skin covering the eye.
After glaucoma shunt surgery, patients prescribed a topical antibiotic for 1-2 weeks and a topic steroid for 4 weeks.
Cyclophotocoagulation (CPC) is a procedure normally performed in the operating room under local anesthesia. It uses laser energy to target the ciliary body epithelial cells, which are the cells within the eye responsible for the production of aqueous fluid. By treating these cells the production of fluid can be reduced and the intraocular pressure is decreased.
A newer version of CPC is called micropulse-CPC (mCPC). Similar to transscleral CPC, mCPC is normally performed in the operating room under local anesthesia. With mCPC, the laser energy is spread out in a more diffuse manner when compared to transscleral CPC. mCPC is effective at lowering the eye pressure and has a lower risk of complications when compared to transscleral CPC. It is often used in advanced disease where the risk of incisional surgery carries a greater risk of permanent vision loss, and for patients that may not be able to tolerate incisional surgery.
After mCPC, patients are prescribed a topical steroid medication for 1-4 weeks.
At Colvard-Kandavel Eye Center, we are committed to providing patients with safe, effective, and innovative options for managing glaucoma. One of the newest therapies now available is the iDose® implant, designed for patients with mild to moderate open-angle glaucoma.
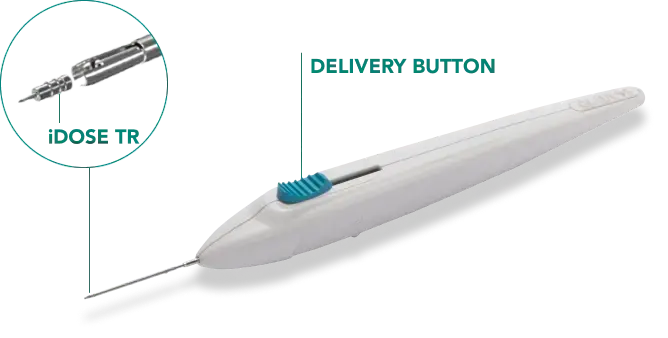
The iDose® is a very small implant placed inside the eye. Once in place, it slowly and steadily releases medication over time. The purpose is to help lower eye pressure—a key factor in protecting vision for people with glaucoma. By doing so, iDose® may reduce or even eliminate the need for daily glaucoma eye drops.
In clinical trials, iDose® was shown to provide greater efficacy than eye drops alone. This is because the implant delivers medication consistently, without the day-to-day challenges of remembering to take drops or applying them correctly. Consistent dosing helps maintain steady eye pressure, which is critical for long-term protection of the optic nerve.
The procedure is performed in the operating room and is often combined with cataract surgery, though it can also be done on its own. A tiny incision is made, through which the iDose® is gently positioned inside the eye. The procedure is typically very quick and less invasive than traditional cataract surgery, which often allows for a slightly faster recovery.
The iDose® procedure carries very low risk overall, particularly when performed at the same time as cataract surgery. It is designed to stay securely in place and release medication gradually, with safety confirmed in multiple clinical studies.
Benefits of iDose®
Our team at Colvard-Kandavel Eye Center is proud to have been directly involved in the clinical studies that led to the approval of iDose®, giving us among the most experience in the nation with this new technology. This early involvement reflects our ongoing commitment to advancing eye care and offering patients the most up-to-date treatments.
Dr. Justin Dredge, our fellowship-trained Glaucoma Specialist, leads our glaucoma program. He is highly experienced with the latest surgical and medical treatments for glaucoma, and his expertise ensures that patients receive thoughtful, individualized care with access to innovative options like iDose®.
Not every patient with glaucoma is a candidate for iDose®. It may be considered for those with mild to moderate open-angle glaucoma who would benefit from more consistent eye pressure control or who have difficulty with daily eye drops.
Like all medical treatments, the iDose® has potential risks and benefits. Our physicians will review your medical history, examine your eyes, and discuss whether this approach is appropriate for your situation. The goal is always the same: protecting your vision and helping you live with glaucoma as comfortably as possible.
Colvard-Kandavel Eye Center offers personalized eye care services for patients with routine and complex eye conditions.
Our team is here to help you make an appointment with the specialists that you need.